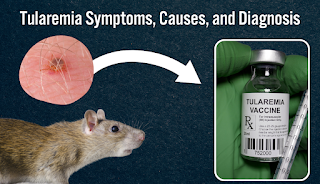
Tularemia Disease: A Rare but Potentially Severe Infectious Disease
Tularemia Disease
Introduction
Tularemia Disease was first identified in 1911 when it caused a tularemia disease outbreak in ground squirrels in Tulare County, California.
The Tularemia, also known as rabbit fever or deer fly fever, is rare. Tularemia potentially severe infectious tularemia disease caused by the bacterium Francisella tularensis. It can affect humans through contact with infected animals, ticks, or contaminated water and soil. Following are the causes, symptoms, diagnosis, treatment, and prevention of tularemia to increase awareness. It is important to understand this rare but important infectious tularemia disease.
Symptoms
The symptoms of Tularemia Disease can depend on the mode of transmission. The following are the most common symptoms of tularemia:
- Fever
- Chills
- Headache
- Muscle aches
- Joint pain
- Fatigue
- Skin rash
- Ulcers at the site of infection
- Swollen lymph nodes
- Difficulty breathing
- Chest pain
- Nausea and vomiting
- Diarrhea
In some cases, tularemia can lead to more severe complications.
Causes Tularemia Disease
The most common modes of transmission of tularemia include:
Tick and deerfly bites: Tularemia Disease can be transmitted to humans through bites from infected ticks or deerflies, which are common in rural areas.
Handling infected animals: People can get infected with tularemia by handling or eating infected animals, such as rabbit fever, rodents, and hares, or by inhaling dust or aerosols contaminated with their feces or urine.
Drinking contaminated water: Tularemia can be transmitted through contaminated water, especially in areas where the bacterium is endemic.
Inhalation of contaminated air: People can get infected with Tularemia Disease by inhaling aerosols containing the bacterium when the bacteria are released during laboratory experiments or bioterrorism attacks.
Transmission
The following are the most common modes of transmission of tularemia:
Tick and deerfly bites: Tularemia can be transmitted to humans through bites from infected ticks or deerflies.
Handling infected animals: The risk of transmission is highest among hunters, trappers, and people who work with animals or soil.
Drinking contaminated water: Tularemia can be transmitted through contaminated water, especially in areas where the bacterium is endemic.
Inhalation of contaminated air: People can get infected with Tularemia Disease by inhaling aerosols containing the bacterium, such as when the bacteria are released during laboratory experiments or bioterrorism attacks.
Diagnosis
Diagnosing tularemia can be challenging due to its nonspecific symptoms and low incidence.
The following tests can be used to diagnose tularemia:
Blood tests: Blood tests can detect antibodies to Francisella tularensis and can be useful in confirming the diagnosis in patients with suspected tularemia.
Culture: Culture of the bacterium from blood, tissue, or other body fluids can confirm the diagnosis of tularemia. However, this method requires specialized laboratory facilities and can take several days to yield results.
Polymerase chain reaction (PCR): PCR can detect the DNA of Francisella tularensis in blood, tissue, or other body fluids and can be useful in early diagnosis and monitoring of treatment response. However, this method requires specialized laboratory facilities and expertise.
Treatment Tularemia Disease
Tularemia is treatable with antibiotics. The following antibiotics are effective against tularemia:
Streptomycin: Streptomycin is the preferred antibiotic for severe cases. The treatment course is usually 10-14 days.
Gentamicin: Gentamicin is an alternative antibiotic for severe cases of tularemia and can be administered intravenously or intramuscularly. The treatment course is usually 10-14 days.
Doxycycline: Doxycycline is an effective antibiotic for mild cases of Tularemia Disease and can be administered orally for 10-14 days.
Ciprofloxacin: Ciprofloxacin is an alternative antibiotic for mild cases. It can be administered orally for 10-14 days.
Prevention and Control
Preventing tularemia involves reducing exposure to infected animals, ticks, and contaminated water and soil. The following measures can be effective in preventing tularemia:
- Avoiding contact with sick or dead animals, especially rabbit fever, rodents, and hares
- Wearing protective clothing, such as gloves, boots, and long sleeves, when handling animals or working in areas where tularemia is endemic
- Using insect repellents containing DEET on exposed skin and clothing to prevent tick and insect bites
- Removing ticks promptly and correctly using tweezers to grasp the tick as close to the skin as possible and pulling it straight out
- Drinking only treated or boiled water and avoiding swimming or wading in contaminated water
- Washing hands thoroughly with soap and water after handling animals or working in areas where tularemia is endemic
- Reporting any suspected cases of tularemia to local health authorities
- Following safe laboratory practices to prevent accidental exposure to Francisella tularensis during laboratory experiments.
Conclusion Tularemia Disease
Preventing Tularemia Disease involves reducing exposure to infected animals, ticks, and contaminated water and soil by following safe practices and taking appropriate precautions.
In summary, tularemia is a rare but potentially severe infectious tularemia disease. It can require prompt diagnosis and treatment to prevent complications and improve outcomes.
Read More: Lymphocytic


.png)